Introduction to Lymphadenoma
Lymphadenoma is a rare, benign tumor that often puzzles both patients and doctors due to its uncommon nature. Found mostly in the salivary glands, particularly the parotid gland, lymphadenoma is a slow-growing, painless mass that can mimic other conditions, making it tricky to diagnose. This tumor combines epithelial cells and lymphoid tissue, creating a unique structure that sets it apart from other growths. While it’s not cancerous, understanding lymphadenoma is crucial for proper treatment and peace of mind. This article dives deep into what lymphadenoma is, its types, causes, symptoms, diagnosis, treatment, and more, using simple language that even school students can grasp. By exploring this topic thoroughly, we aim to shed light on this lesser-known condition and provide clear, reliable information to help you understand lymphadenoma and its impact.
Understanding Lymphadenoma
Lymphadenoma is a benign tumor, meaning it’s non-cancerous and doesn’t spread to other parts of the body. It most commonly appears in the parotid gland, located near the jaw and ear, but can occasionally occur in other areas like the submandibular gland, neck, or oral cavity. The term “lymphadenoma” refers to its makeup: a mix of epithelial cells (which form the gland’s structure) and lymphoid tissue (similar to what’s found in lymph nodes). This combination gives lymphadenoma its distinctive appearance under a microscope. There are two main types: sebaceous lymphadenoma, which contains oil-producing sebaceous cells, and non-sebaceous lymphadenoma, which lacks these cells. Both types are rare, with fewer than 100 cases reported in medical literature. Lymphadenoma typically affects older adults, with a median age of around 65, though it can occur in children and younger adults too.
Types of Lymphadenoma
Lymphadenoma comes in two primary forms: sebaceous and non-sebaceous. Sebaceous lymphadenoma is characterized by the presence of sebaceous cells, which produce a fatty substance similar to skin oils. These tumors are often found in the parotid gland and are slightly more common in men. Non-sebaceous lymphadenoma, on the other hand, lacks these sebaceous cells and shows a wider range of cell types, such as basaloid or squamous cells. This type is more common in women and can appear outside the parotid gland, like in the neck or oral cavity. Both types of lymphadenoma are benign, but their different cellular makeup can affect how they look under a microscope and how doctors diagnose them. Understanding these types helps in tailoring the right treatment approach and distinguishing lymphadenoma from other similar tumors.
Causes and Risk Factors of Lymphadenoma
The exact cause of lymphadenoma remains unclear, as research on this rare tumor is limited. However, some studies suggest that lymphadenoma may develop from abnormal growth within salivary gland tissue, possibly linked to changes in lymph nodes embedded in the gland. About 30% of patients with lymphadenoma have a history of immunosuppressive therapy for unrelated conditions, which might play a role in its development, though the connection isn’t fully understood. Unlike some cancers, lymphadenoma isn’t strongly tied to genetics or lifestyle factors like smoking or diet. It affects both men and women, with no clear gender preference, and can occur across a wide age range, from children to the elderly. Environmental factors or infections, such as HPV or EBV, have not been linked to lymphadenoma, making its origins a bit of a mystery.
Symptoms of Lymphadenoma
Lymphadenoma typically presents as a painless, slow-growing mass, often in the parotid gland near the ear or jaw. The lump is usually well-defined, encapsulated, and ranges from 0.6 to 6 cm in size, with an average of about 2.2 cm. Patients might notice a firm or soft bump that doesn’t cause discomfort, which is why lymphadenoma is often mistaken for other benign tumors like pleomorphic adenoma or Warthin’s tumor. In rare cases, it may cause slight tenderness or swelling, but symptoms like pain, facial nerve weakness, or rapid growth are uncommon and could suggest a different condition. Because lymphadenoma grows slowly, it might go unnoticed for years. If you feel a persistent lump in your neck, jaw, or mouth area, it’s worth checking with a doctor to rule out lymphadenoma or other issues.
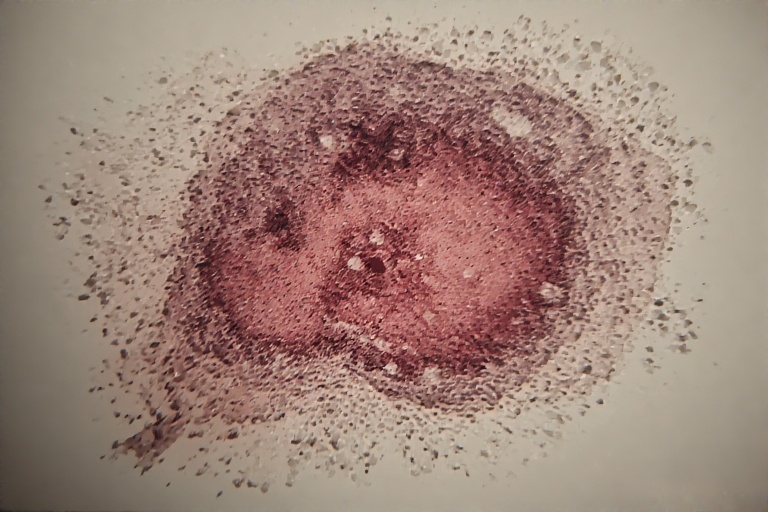
Diagnosis of Lymphadenoma
Diagnosing lymphadenoma can be challenging because it resembles other salivary gland tumors. Doctors start with a physical exam, feeling for a lump in the neck or jaw area. Imaging tests, like CT scans or MRIs, help determine the tumor’s size and location, but they can’t confirm lymphadenoma definitively. A fine needle aspiration (FNA) biopsy, where a small sample of the tumor is taken with a needle, is often used but may not always provide a clear diagnosis due to lymphadenoma’s unique structure. The gold standard is a surgical biopsy, where the tumor is removed and examined under a microscope. Pathologists look for a mix of epithelial and lymphoid cells, with or without sebaceous differentiation, to confirm lymphadenoma. Immunohistochemistry, which tests for specific proteins like CK7 or p63, helps distinguish it from similar tumors.
Treatment Options for Lymphadenoma
The primary treatment for lymphadenoma is surgical removal, which is usually curative. A procedure called superficial parotidectomy is common when the tumor is in the parotid gland, as it removes the mass while preserving important structures like the facial nerve. Since lymphadenoma is benign, complete removal typically prevents recurrence, and no further treatment is needed. In rare cases, if the tumor transforms into a malignant form (like sebaceous or basal cell adenocarcinoma), additional treatments like radiation may be considered, but this is extremely uncommon. Surgery is generally low-risk, and patients recover well, with follow-up studies showing no recurrence in most cases after 1–8 years. If lymphadenoma is suspected, a skilled surgeon and pathologist are key to ensuring accurate diagnosis and treatment, minimizing complications, and maintaining quality of life post-surgery.
Prognosis and Outcomes
The prognosis for lymphadenoma is excellent because it’s a benign tumor. After surgical removal, most patients experience no recurrence, and the tumor doesn’t spread to other parts of the body. Studies following patients for up to 8 years show that lymphadenoma rarely comes back after complete excision. In very rare cases, malignant transformation into cancers like sebaceous lymphadenocarcinoma has been reported, but this is an exception, not the rule. Patients generally enjoy a good quality of life after treatment, with minimal complications if the surgery is done carefully to avoid damaging nearby nerves. Regular follow-up with a doctor is recommended to monitor for any changes, but for most people, lymphadenoma is a one-time issue that’s resolved with surgery. Awareness and early detection are key to keeping outcomes positive.
Differentiating Lymphadenoma from Other Conditions
Lymphadenoma is often mistaken for other salivary gland tumors due to its appearance. Conditions like Warthin’s tumor, pleomorphic adenoma, mucoepidermoid carcinoma, or even lymphoepithelial cysts can look similar on imaging or initial biopsy. Unlike malignant tumors, lymphadenoma lacks signs of aggressive growth, such as invasion into nearby tissues or rapid enlargement. Pathologists use specific markers, like the absence of HPV, EBV, or HHV-8, and the presence of basal cell markers (p63, CK5/6) to confirm lymphadenoma. The lymphoid stroma, which looks like reactive lymph node tissue with germinal centers, is another clue. Misdiagnosis can lead to unnecessary worry or treatment, so expert pathological analysis is critical. For school students, think of lymphadenoma as a unique puzzle piece that doctors must carefully identify among similar-looking pieces.
Research and Future Directions
Research on lymphadenoma is limited due to its rarity, but ongoing studies aim to clarify its causes and improve diagnosis. Scientists are exploring whether lymphadenoma arises from lymph nodes within the salivary gland or from the gland tissue itself. Advances in immunohistochemistry and molecular testing may make it easier to distinguish lymphadenoma from other tumors, reducing misdiagnoses. There’s also interest in understanding why some patients on immunosuppressive therapy develop lymphadenoma, which could point to immune system links. Future research might uncover genetic or environmental factors that contribute to its formation, though no such links exist yet. For now, raising awareness about lymphadenoma among doctors and patients is crucial, as it’s often overlooked in standard medical texts. Continued studies will help ensure better outcomes for those affected by this rare condition.
Living with Lymphadenoma
For those diagnosed with lymphadenoma, the journey is usually straightforward. Since the tumor is benign, surgery is often the only step needed, and recovery is typically smooth. Patients may feel anxious about a lump or the idea of surgery, but understanding that lymphadenoma is non-cancerous can ease worries. After surgery, most people return to normal activities within weeks, with minimal scarring or complications if the procedure is done by an experienced surgeon. Regular check-ups are recommended to ensure the tumor doesn’t return, though this is rare. If you notice a lump that doesn’t go away, don’t panic—see a doctor for a proper evaluation. For students, think of lymphadenoma as a rare, treatable bump that doctors can handle with care, letting you get back to your daily life quickly.
FAQs About Lymphadenoma
What is lymphadenoma, and is it dangerous?
Lymphadenoma is a rare, benign tumor usually found in the salivary glands, especially the parotid gland. It’s not dangerous because it doesn’t spread or turn cancerous in most cases. Surgical removal is typically all that’s needed for treatment.
How do doctors diagnose lymphadenoma?
Doctors use physical exams, imaging tests like CT scans, and biopsies to diagnose lymphadenoma. A surgical biopsy, examined under a microscope, is the most reliable way to confirm it, as lymphadenoma can look like other tumors.
Can lymphadenoma come back after surgery?
Lymphadenoma rarely recurs after complete surgical removal. Follow-up studies show no recurrence in most patients after 1–8 years, making surgery a highly effective treatment.
Who is at risk for developing lymphadenoma?
Lymphadenoma can affect anyone, from children to older adults, with a median age of 65. About 30% of patients have a history of immunosuppressive therapy, but no clear risk factors like genetics or infections are known.
How is lymphadenoma different from lymphoma?
Lymphadenoma is a benign salivary gland tumor, while lymphoma is a cancer of the lymphatic system. Lymphadenoma doesn’t spread and is treated with surgery, whereas lymphoma may require chemotherapy or radiation.
Conclusion
Lymphadenoma is a rare but fascinating condition that highlights the complexity of the human body. As a benign tumor primarily affecting the salivary glands, lymphadenoma is treatable with surgery and carries an excellent prognosis. By understanding its types, symptoms, and diagnosis, patients and students alike can demystify this uncommon condition. Though research is ongoing, lymphadenoma remains a manageable issue with proper medical care. If you suspect a lump could be lymphadenoma, consult a healthcare provider for peace of mind and effective treatment. This guide aims to empower you with clear, accessible knowledge about lymphadenoma, ensuring you’re well-informed about this rare but treatable tumor.